The Sequence 10/31-11/6
23andme to Detect Breast Cancer Susceptibility, Genes Associated with Dyslexia, The Inflation Reduction Act and Healthcare Costs, NYC Partnership to Study Utility of Expanded Newborn Screening
23andme to detect breast cancer susceptibility
As many are aware, the direct-to-consumer genetic testing company 23andme offers the ability to test for inherited risks for several health conditions. This includes testing for mutations, or harmful changes in the DNA, that cause an increased susceptibility to breast and ovarian cancers. Here, I summarize an article by Today’s Sarah Jacoby on exactly what 23andme tests for in the BRCA genes.
Is 23andme accurate in detecting my risk for breast cancer?
23andme is accurate in identifying the mutations it tests for. That’s the catch. Although there are more than 1,000 possible mutations in BRCA1 and BRCA2 that could affect cancer risk, 23andme is only testing for three.
Why only three?
They’re the most common. 23andme tests for what we call the ‘founder mutations’ in BRCA1 and BRCA2. A founder mutation occurs when a group of people is culturally or geographically isolated, therefore sharing a large portion of their DNA. These three founder mutations are the most common in the general population, and in the Ashkenazi Jewish population in particular, with a carrier rate of 1 in 40 in the Ashkenazi Jewish population.
What about all of the other potential mutations you mentioned?
They’re not being tested for. Not only are other BRCA1 and BRCA2 mutations not being looked at, but there are several other genes that cause increased risks for breast and ovarian cancer that 23andme is not analyzing.
What’s the takeaway?
The takeaway is that 23andme is accurate, but not all-inclusive. If you have a family history of breast or ovarian cancer, or feel you need more comprehensive testing to understand your inherited risks for cancer, you should consider speaking to a genetic counselor about what testing options make the most sense for you.
New genes associated with dyslexia identified
Doust et al. studied the genome (entire set of DNA) of 51,800 adults from 23andme’s dataset who self-reported a dyslexia diagnosis. The purpose was to identify whether there are certain changes in the DNA that are linked with dyslexia.
How did they do that?
GWAS.
What?
GWAS, or Genome-wide association studies, look at the genome of a large group of people, searching for small genetic variations called single nucleotide polymorphisms (aka SNPs). GWAS look for SNPs associated with certain traits. An example for this study would be, “look, there’s a common SNP in individuals with dyslexia that’s not in the individuals without dyslexia”.
The results?
There are a few interesting results!
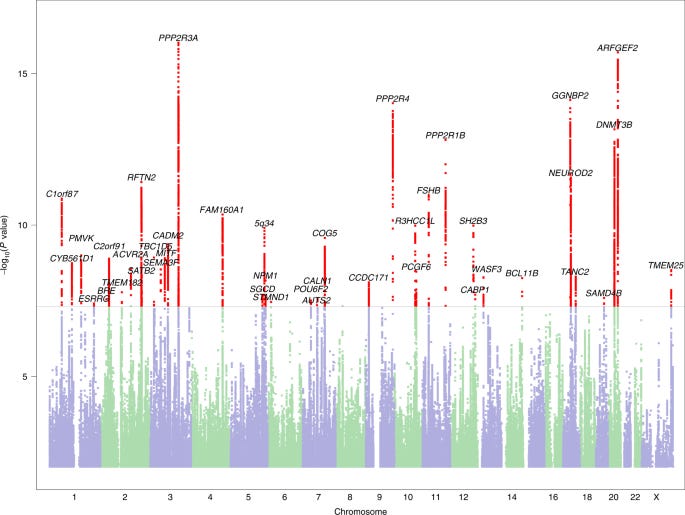
The team identified 42 SNPs that are significantly associated with dyslexia (below).
Photo credit: Nature Genetics
There was increased association in genes expressed in the frontal cortex, cortex and anterior cingulate cortex of the brain (i.e. parts of the brain in charge of processing information and emotions as well as decision-making).
Dyslexia diagnoses were negatively correlated with quantitative reading and spelling measures (i.e. rates of dyslexia increased as reading and spelling scores decreased), and positively correlated with ADHD, work in vocational-related areas, jobs involving heavy and manual work, ambidexterity (i.e. equal use of left and right hand), pain perception, and hearing difficulties.
Interesting. What’s the takeaway here?
There may be more genetic and inherited associations with dyslexia than previously thought. With further studies, significant genetic mutations identified in research like this can be used to create polygenic risk scores, or numbers that estimates one’s risk for dyslexia based on their DNA. This type of risk score could contribute to earlier detection and treatment of children with dyslexia.
How The Inflation Reduction Act could affect healthcare costs
The Inflation Reduction Act of 2022 (IRA), signed into law by President Joe Biden on August 16, 2022, has some lofty goals in order to decrease inflation in the U.S.. Those include reducing the Federal budget deficit, lowering prescription drug prices, and investing into clean, domestic energy production.
Great, so this should lower drug prices and healthcare costs, right?
Yes, but it’s complicated. This act will certainly lower out of pocket costs of prescription drugs for consumers. However, someone will need to cover those prescription drug costs, so who will it be?
Well, it will be the responsibility of prescription drug manufacturers.
How will that work?
In three ways. Firstly, through inflation-based rebates. If prescription drug companies increase drug prices at a rate that exceeds the rate of inflation, the difference must be given back to Medicare as a rebate. It’s basically a penalty on drug companies for charging too much.
Secondly, through Medicare part D redesign. This means prescription drug manufacturers will be required to cover 25% of the cost of drugs that was historically payed for by Medicare.
Thirdly, through Medicare price negotiations. Health and Human Services (HHS) will be able to regulate prices of certain drugs. HHS will be able to tell manufacturers what they are willing to pay toward the drugs, and companies that don’t comply will be fined.
This all sounds like it saves consumers money. Good, right?
These plans do save consumers money in the immediate future, upon implementation of these laws. However, concerns come in when we think about how the prescription drug manufacturers and insurance companies, who will be making much less profit than they were before, will fare in all of this and what might happen.
Since insurance companies will be paying out more, they may start limiting the amount of individuals they will cover medications for, decreasing access.
Since prescription drug manufacturers will be paying out more, manufacturers as well as pharmaceutical companies innovating these new drugs will have less money available for research and development, to come out with new treatments for conditions. Also, meaning less access for patients to receive healthcare.
Interesting. What’s the takeaway?
The takeaway is, we’ll see what happens. It’s great that out of pocket costs will be lower for patients in the initial steps of this program, but we will need to see how this shift in cost responsibility affects the drug market in general.
Credit for this one also goes to a fellow Substack writer for this post. Visit BowTiedBiotech here:
Major NYC partnership to study utility of expanded newborn screening
Columbia University Irving Medical Center, NewYork-Presbyterian, the New York State Department of Health, Sema4, and Illumina have joined together to participate in a newborn screening study in New York City called GUARDIAN, which stands for Genomic Uniform-screening Against Rare Diseases in All Newborns.
How does newborn screening work now?
Newborn screening (NBS) is a routine procedure for which babies are given a prick to their heels 24-48 hours after they’re born to collect a blood sample. That sample is used to test for a number of rare, severe genetic disorders that have effective treatments. Think metabolic disorders, endocrine disorders, hemoglobinopathies, and other enzyme deficiencies that can prevent babies from feeding properly, for example. The main goal is to prevent infant death in the case of a disorder that went undetected before birth.
Standard newborn screening covers anywhere from ~30-70 genetic conditions. The number of diseases screened for varies by state. Generally, in order for a condition to be included on the newborn screen panel, it has to have an intervention that is considered life-altering or lifesaving.
Cool. What are they studying?
The study will look at the utility of screening newborns for up to 250 rare genetic conditions that are not covered by standard newborn screening. They will screen 100,000 babies born in one of NewYork-Presbyterian's hospitals in New York City for 250 rare genetic conditions in order to see if adding these conditions to NBS does in fact drive earlier diagnosis and treatment for more babies.
Another important question the study will try and answer is the utility of whole genome sequencing (WGS), or technology that sequences all of the DNA, in NBS. The study will utilize whole genome sequencing provided by GeneDx. Current NBS uses some genetic testing, but mostly relies on tandem mass spectrometry (MS/MS) or high pressure liquid chromatography (HPLC), which are ways to identify abnormal levels of amino acids that could be indicative of metabolic disorders.
What’s the takeaway?
Dr. Paul Kruszka, Chief Medical Officer of GeneDx at Sema4, elaborates on the vision of the study here:
By being able to intervene in the healthcare of more children with rare disease, we have the opportunity to improve and extend more lives.